Liposomalni Imuno C,D3,Cink
 Objavljeno: 23. 08. 2022 - 11:03
Objavljeno: 23. 08. 2022 - 11:03 SINERGIJSKO DJELOVANJE VITAMINA C, D3 I CINKA KOD VIRUSNIH INFEKCIJA
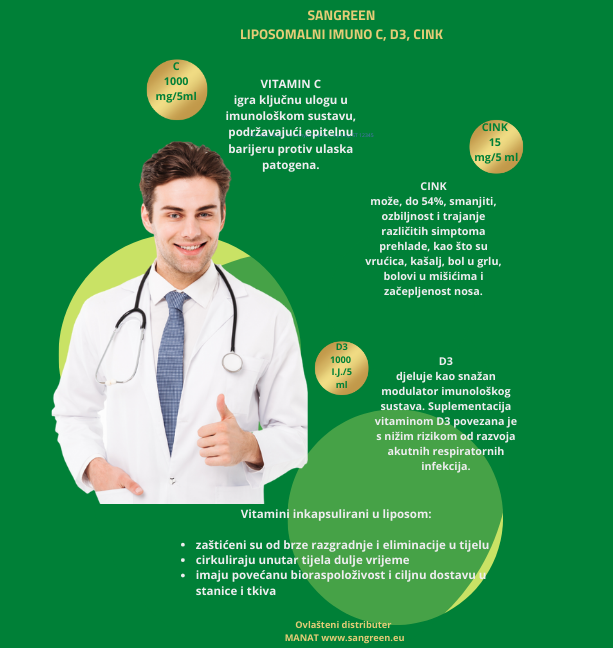
Vitamni C, D3 i cink imaju sinergijsko djelovanje važno za aktivnost imunološkog sustava, posebice kod virusnih infekcija. Medicinska literatura pokazuje da suplementacija cinkom, vitaminom C i D3 može ublažiti virusne respiratorne infekcije. Pri kontaktu s virusom nastaje povećana potražnja organizma za ovim nutrijentima jer su ključni za početak imunološkog odgovora, kao i za smanjenje rizika od ozbiljnog napredovanja virusne infekcije.
Cink
Cink je neophodan za funkciju i cjelovitost imunološkog sustava (33), a također igra važnu ulogu u radu epitelnih barijera, koje sprječavaju ulazak virusa i bakterija u organizam (34-37).
Cink ima izravno antivirusno djelovanje, što ga čini esencijalnim za imunološki odgovor na virusnu infekciju (31, 32).
Nedostatak cinka pogađa otprilike jednu trećinu svjetske populacije (56) i smatra se globalnim prehrambenim problemom koji pogađa sve skupine stanovništva u razvijenim i zemljama u razvoju.
Kliničke studije su pokazale da suplementacija cinkom može za do 54% smanjiti ozbiljnost i trajanje različitih simptoma prehlade, kao što su vrućica, kašalj, bol u grlu, bolovi u mišićima i začepljenost nosa (90-92), koji se također mogu pojaviti nakon infekcije SARS-CoV-2.

Vitamin C
Vitamin C ima snažna antioksidativna i antihistaminska svojstva (19, 95, 96. 108). Naše tijelo ne proizvodi vitamin C stoga je nophodno uzimati ga kroz hranu ili suplemente.
Meta-analiza 44 studije utvrdila je da suplementacija vitaminom C smanjuje trajanje obične prehlade kod odraslih i djece i smanjuje ozbiljnosti simptoma, što je povezano s ulogom ovog vitamina u funkciji imunološkog sustava (107). Također je utvrđeno da primjena vitamina C smanjuje respiratorne simptome upale pluća kod kritično bolesnih pacijenata (109).
Starija populacija posebno je pogođena nedostatkom vitamina C jer u ovoj skupini prevladavaju kronične ili akutne bolesti (100-103). Na primjer, niske razine vitamina C (≤ 17 μmol/L) u populaciji britanskih starijih osoba bile su povezane sa svim uzrocima smrtnosti, uključujući kardiovaskularne uzroke (104).
Vitamin D
Unatoč tradicionalnom nazivu, vitamin D zapravo je hormon, budući da osim što se proizvodi endogeno, djeluje na regulaciju više od 200 gena u različitim tipovima stanica (125-127).
Uz svoje klasične učinke na homeostazu kalcija i održavanje zdravlja kostiju, vitamin D3 igra važnu ulogu u imunološkoj funkciji tijela (17, 19, 134–136). On zapravo djeluje kao snažan modulator imunološkog sustava i ima receptore u svim imunološkim stanicama. Osim imunoloških stanica, receptor vitamina D3 također se nalazi u plućnim epitelnim stanicama.
Meta-analiza 25 randomiziranih kontroliranih studija pokazala je da je suplementacija vitaminom D3 povezana s nižim rizikom od razvoja akutnih respiratornih infekcija.
Neka istraživanja sugeriraju da postoji korelacija između nedostatka vitamina D i osjetljivosti na infekciju SARS-CoV-2 i ozbiljnosti bolesti (24, 106, 140, 148-152). Ilie i sur. (149) pronašli su negativnu korelaciju između prosječne razine vitamina D u serumu u 20 europskih zemalja i broja oboljelih od COVID-19 i mortaliteta na milijun stanovnika. Slično tome, kasnija studija s izraelskom kohortom od 7807 ispitanika identificirala je značajno niže razine vitamina D među onima koji su bili pozitivni na COVID-19 u usporedbi s onima koji su bili negativni.
Liposomalni oblik povećava apsorpciju i bioraspoloživost
Nutrijenti inkapsulirani u liposom zbog veličine liposoma od 200 nm i ovojnice od fosfolipida, zaštićeni su od brze razgradnje i eliminacije u tijelu, porlaze nepromijenjeni kroz probavni trakt i apsorbiraju se u tankom crijevu. Zato mogu cirkulirati unutar tijela dulje vrijeme, što povećava vjerojatnost da će aktivna tvar ući u ciljna tkiva i stanice.
Studije otkrivaju da liposomi povečavaju bioraspoloživost nutrijenata i njihovu ciljnu dostavu u tkiva i stanice kojima su potrebni.
Sangreen liposomalni Imuno C, D3, cink sinergijski djeluje na optimalan rad imunološkog sustava i daje snažnu podršku kod virusnih infekcija i prehada. Ne sadrži alkohol te je siguran za djecu. Pakiranje od 250 ml uz dozranje od 5 ml dnevno dostatno je za 50 dana korištenja.
Literatura:
1. Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients. (2020) 12:1181 10.3390/nu12041181 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Infusino F, Marazzato M, Mancone M, Fedele F, Mastroianni CM, Severino P, et al.. Diet supplementation, probiotics, and nutraceuticals in SARS-CoV-2 infection: a scoping review. Nutrients. (2020) 12:1718. 10.3390/nu12061718 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. Jaggers GK, Watkins BA, Rodriguez RL. COVID-19: repositioning nutrition research for the next pandemic. Nutr Res. (2020) 81:1–6. 10.1016/j.nutres.2020.07.005 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al.. Coronavirus disease 2019-COVID-19. Clin Microbiol Rev. (2020) 33:e00028–20. 10.1128/CMR.00028-20 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. (2020) 109:102433. 10.1016/j.jaut.2020.102433 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, et al.. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. (2020) 5:536–44. 10.1038/s41564-020-0695-z [PMC free article] [PubMed] [CrossRef] [Google Scholar]
7. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al.. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. 10.1038/s41586-020-2012-7 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Caccialanza R, Laviano A, Lobascio F, Montagna E, Bruno R, Ludovisi S, et al.. Early nutritional supplementation in non-critically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): Rationale and feasibility of a shared pragmatic protocol. Nutrition. (2020) 74:110835. 10.1016/j.nut.2020.110835 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
9. Dhama K, Patel SK, Pathak M, Yatoo MI, Tiwari R, Malik YS, et al.. An update on SARS-CoV-2/COVID-19 with particular reference to its clinical pathology, pathogenesis, immunopathology and mitigation strategies. Travel Med Infect Dis. (2020) 37:101755. 10.1016/j.tmaid.2020.101755 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Wu D, Lewis ED, Pae M, Meydani SN. Nutritional modulation of immune function: analysis of evidence, mechanisms, and clinical relevance. Front Immunol. (2018) 9:3160. 10.3389/fimmu.2018.03160 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Childs CE, Calder PC, Miles EA. Diet and immune function. Nutrients. (2019) 11:1933. 10.3390/nu11081933 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
12. Cohen J. Saving lives without new drugs. Science. (2014) 346:911. 10.1126/science.346.6212.911 [PubMed] [CrossRef] [Google Scholar]
13. Ferrara F, De Rosa F, Vitiello A. The central role of clinical nutrition in COVID-19 patients during and after hospitalization in intensive care unit. SN Compr Clin Med. (2020) 11:1–5. 10.1007/s42399-020-00410-0 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Laviano A, Koverech A, Zanetti M. Nutrition support in the time of SARS-CoV-2 (COVID-19). Nutrition. (2020) 74:110834. 10.1016/j.nut.2020.110834 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Naja F, Hamadeh R. Nutrition amid the COVID-19 pandemic: a multi-level framework for action. Eur J Clin Nutr. (2020) 74:1117–21. 10.1038/s41430-020-0634-3 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Romano L, Bilotta F, Dauri M, Macheda S, Pujia A, De Santis GL, et al.. Short report - medical nutrition therapy for critically ill patients with COVID-19. Eur Rev Med Pharmacol Sci. (2020) 24:4035–9. 10.26355/eurrev_202004_20874 [PubMed] [CrossRef] [Google Scholar]
17. Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients. (2020) 12:236. 10.3390/nu12010236 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Jayawardena R, Sooriyaarachchi P, Chourdakis M, Jeewandara C, Ranasinghe P. Enhancing immunity in viral infections, with special emphasis on COVID-19: a review. Diabetes Metab Syndr. (2020) 14:367–82. 10.1016/j.dsx.2020.04.015 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
19. Jovic TH, Ali SR, Ibrahim N, Jessop ZM, Tarassoli SP, Dobbs TD, et al.. Could vitamins help in the fight against COVID-19? Nutrients. (2020) 12:2550. 10.3390/nu12092550 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
20. Messina G, Polito R, Monda V, Cipolloni L, Di Nunno N, Di Mizio G, et al.. Functional role of dietary intervention to improve the outcome of covid-19: a hypothesis of work. Int J Mol Sci. (2020) 21:3104. 10.3390/ijms21093104 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
21. Johnston CS, Barkyoumb GM, Schumacher SS. Vitamin C supplementation slightly improves physical activity levels and reduces cold incidence in men with marginal vitamin C status: a randomized controlled trial. Nutrients. (2014) 6:2572–83. 10.3390/nu6072572 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Sanchez J, Villada OA, Rojas ML, Montoya L, Diaz A, Vargas C, et al.. Effect of zinc amino acid chelate and zinc sulfate in the incidence of respiratory infection and diarrhea among preschool children in child daycare centers. Biomedica. (2014) 34:79–91. 10.1590/S0120-41572014000100011 [PubMed] [CrossRef] [Google Scholar]
23. Lassi ZS, Moin A, Bhutta ZA. Zinc supplementation for the prevention of pneumonia in children aged 2 months to 59 months. Cochrane Database Syst Rev. (2016) 12:CD005978. 10.1002/14651858.CD005978.pub3 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. (2020) 12:988 10.3390/nu12040988 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
25. Name JJ, Vasconcelos AR, Souza ACR, Favaro WJ. Vitamin D. Zinc Glutamine: Synergistic Action with OncoTherad Immunomodulator in Interferon Signaling COVID-19. (2020). SSRN; Available online at: 10.2139/ssrn.3650249 (accessed August 25, 2020). [CrossRef] [Google Scholar]
26. Ames BN. Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. Proc Natl Acad Sci USA. (2006) 103:17589–94. 10.1073/pnas.0608757103 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
27. Brock WH. Justus von Liebig: The Chemical Gatekeeper. Cambridge: Cambridge University Press; (2002). [Google Scholar]
28. Davidson EA, Howarth RW. Environmental science: nutrients in synergy. Nature. (2007) 449:1000–1. 10.1038/4491000a [PubMed] [CrossRef] [Google Scholar]
29. Kaspari M, Powers JS. Biogeochemistry and geographical ecology: embracing all twenty-five elements required to build organisms. Am Nat. (2016) 188(Suppl. 1):S62–73. 10.1086/687576 [PubMed] [CrossRef] [Google Scholar]
30. Bauer SR, Kapoor A, Rath M, Thomas SA. What is the role of supplementation with ascorbic acid, zinc, vitamin D, or N-acetylcysteine for prevention or treatment of COVID-19? Cleve Clin J Med. (2020). 10.3949/ccjm.87a.ccc046. [Epub ahead of print]. [PubMed] [CrossRef] [Google Scholar]
31. Brewer J, Gomez Marti JL, Brufsky A. Potential interventions for SARS-CoV-2 infections: zinc showing promise. J Med Virol. (2020). 10.1002/jmv.26523. [Epub ahead of print]. [PubMed] [CrossRef] [Google Scholar]
32. Hoang BX, Han B. A possible application of hinokitiol as a natural zinc ionophore and anti-infective agent for the prevention and treatment of COVID-19 and viral infections. Med Hypotheses. (2020) 145:110333. 10.1016/j.mehy.2020.110333 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. Maggini S, Wenzlaff S, Hornig D. Essential role of vitamin C and zinc in child immunity and health. J Int Med Res. (2010) 38:386–414. 10.1177/147323001003800203 [PubMed] [CrossRef] [Google Scholar]
34. Sturniolo GC, Fries W, Mazzon E, Di Leo V, Barollo M, D'Inca R. Effect of zinc supplementation on intestinal permeability in experimental colitis. J Lab Clin Med. (2002) 139:311–5. 10.1067/mlc.2002.123624 [PubMed] [CrossRef] [Google Scholar]
35. Shin K, Fogg VC, Margolis B. Tight junctions and cell polarity. Annu Rev Cell Dev Biol. (2006) 22:207–35. 10.1146/annurev.cellbio.22.010305.104219 [PubMed] [CrossRef] [Google Scholar]
36. Finamore A, Massimi M, Conti Devirgiliis L, Mengheri E. Zinc deficiency induces membrane barrier damage and increases neutrophil transmigration in Caco-2 cells. J Nutr. (2008) 138:1664–70. 10.1093/jn/138.9.1664 [PubMed] [CrossRef] [Google Scholar]
37. Maares M, Haase H. Zinc and immunity: An essential interrelation. Arch Biochem Biophys. (2016) 611:58–65. 10.1016/j.abb.2016.03.022 [PubMed] [CrossRef] [Google Scholar]
38. Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: An overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. (2020) 53:25–32. 10.1016/j.cytogfr.2020.05.003 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
39. Rahman MT, Idid SZ. Can Zn Be a Critical Element in COVID-19 Treatment? Biol Trace Elem Res. (2020). 10.1007/s12011-020-02194-9. [Epub ahead of print]. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Skalny AV, Rink L, Ajsuvakova OP, Aschner M, Gritsenko VA, Alekseenko SI, et al.. Zinc and respiratory tract infections: perspectives for COVID19 (Review). Int J Mol Med. (2020) 46:17–26. 10.3892/ijmm.2020.4575 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
41. Truong-Tran AQ, Carter J, Ruffin R, Zalewski PD. New insights into the role of zinc in the respiratory epithelium. Immunol Cell Biol. (2001) 79:170–7. 10.1046/j.1440-1711.2001.00986.x [PubMed] [CrossRef] [Google Scholar]
42. Prasad AS. Zinc: mechanisms of host defense. J Nutr. (2007) 137:1345–9. 10.1093/jn/137.5.1345 [PubMed] [CrossRef] [Google Scholar]
43. Korant BD, Kauer JC, Butterworth BE. Zinc ions inhibit replication of rhinoviruses. Nature. (1974) 248:588–90. 10.1038/248588a0 [PubMed] [CrossRef] [Google Scholar]
44. Suara RO, Crowe JE, Jr. Effect of zinc salts on respiratory syncytial virus replication. Antimicrob Agents Chemother. (2004) 48:783–90. 10.1128/aac.48.3.783-790.2004 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
45. te Velthuis AJ, van den Worm SH, Sims AC, Baric RS, Snijder EJ, van Hemert MJ. Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog. (2010) 6:e1001176. 10.1371/journal.ppat.1001176 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
46. Wei Z, Burwinkel M, Palissa C, Ephraim E, Schmidt MF. Antiviral activity of zinc salts against transmissible gastroenteritis virus in vitro. Vet Microbiol. (2012) 160:468–72. 10.1016/j.vetmic.2012.06.019 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Kaushik N, Anang S, Ganti KP, Surjit M. Zinc: a potential antiviral against hepatitis E virus infection? DNA Cell Biol. (2018) 37:593–9. 10.1089/dna.2018.4175 [PubMed] [CrossRef] [Google Scholar]
48. Read SA, Obeid S, Ahlenstiel C, Ahlenstiel G. The Role of Zinc in Antiviral Immunity. Adv Nutr. (2019) 10:696–710. 10.1093/advances/nmz013 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
49. Lanke K, Krenn BM, Melchers WJ, Seipelt J, van Kuppeveld FJ. PDTC inhibits picornavirus polyprotein processing and RNA replication by transporting zinc ions into cells. J Gen Virol. (2007) 88(Pt 4):1206–17. 10.1099/vir.0.82634-0 [PubMed] [CrossRef] [Google Scholar]
50. Cakman I, Kirchner H, Rink L. Zinc supplementation reconstitutes the production of interferon-alpha by leukocytes from elderly persons. J Interferon Cytokine Res. (1997) 17:469–72. 10.1089/jir.1997.17.469 [PubMed] [CrossRef] [Google Scholar]
51. Berg K, Bolt G, Andersen H, Owen TC. Zinc potentiates the antiviral action of human IFN-alpha tenfold. J Interferon Cytokine Res. (2001) 21:471–4. 10.1089/10799900152434330 [PubMed] [CrossRef] [Google Scholar]
52. Foster M, Samman S. Zinc and regulation of inflammatory cytokines: implications for cardiometabolic disease. Nutrients. (2012) 4:676–94. 10.3390/nu4070676 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
53. McCarty MF, DiNicolantonio JJ. Nutraceuticals have potential for boosting the type 1 interferon response to RNA viruses including influenza and coronavirus. Prog Cardiovasc Dis. (2020) 63:383–5. 10.1016/j.pcad.2020.02.007 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
54. Speth R, Carrera E, Jean-Baptiste M, Joachim A, Linares A. Concentration-dependent effects of zinc on angiotensin-converting enzyme-2 activity (1067.4). FASEB J. (2014) 28:1067.1064 10.1096/fasebj.28.1_supplement.1067.4 [CrossRef] [Google Scholar]
55. McPherson SW, Keunen JE, Bird AC, Chew EY, van Kuijk FJ. Investigate oral zinc as a prophylactic treatment for those at risk for COVID-19. Am J Ophthalmol. (2020) 216:A5–6. 10.1016/j.ajo.2020.04.028 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
56. World Health Organization Childhood and Maternal Undernutrition (2002). Chapter 4. Available online at: https://www.who.int/whr/2002/chapter4/en/index3.html (accessed April 17, 2020).
57. Bailey RL, West KP, Jr, Black RE. The epidemiology of global micronutrient deficiencies. Ann Nutr Metab. (2015) 66(Suppl. 2):22–33. 10.1159/000371618 [PubMed] [CrossRef] [Google Scholar]
58. Prasad AS. Discovery of human zinc deficiency and studies in an experimental human model. Am J Clin Nutr. (1991) 53:403–12. [PubMed] [Google Scholar]
59. do Nascimento Nogueira N, Parente JV, Cozzolino SMF. Mudanças na concentração plasmática de zinco e ácido fólico em adolescentes grávidas submetidas a diferentes esquemas de suplementação Changes in plasma zinc and folic acid. Cad. Saúde pública. (2003) 19:155–60. 10.1590/S0102-311X2003000100017 [PubMed] [CrossRef] [Google Scholar]
60. Chaffee BW, King JC. Effect of zinc supplementation on pregnancy and infant outcomes: a systematic review. Paediatr Perinat Epidemiol. (2012) 26(Suppl. 1):118–37. 10.1111/j.1365-3016.2012.01289.x [PMC free article] [PubMed] [CrossRef] [Google Scholar]
61. Wessels I, Rolles B, Rink L. The potential impact of zinc supplementation on COVID-19 pathogenesis. Front Immunol. (2020) 11:1712. 10.3389/fimmu.2020.01712 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
62. Arumugam VA, Thangavelu S, Fathah Z. COVID-19 and the world with co-morbidities of heart disease, hypertension and diabetes. J Pure Appl Microbiol. (2020) 14:1623–38. 10.22207/JPAM.14.3.01 [CrossRef] [Google Scholar]
63. Dhama K, Patel SK, Kumar R, Rana J, Yatoo MI, Kumar A, et al.. Geriatric population during the COVID-19 pandemic: problems, considerations, exigencies, and beyond. Front Public Health. (2020) 8:574198. 10.3389/fpubh.2020.574198 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
64. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. 10.1001/jama.2020.1585 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
65. Chen MD, Lin PY, Lin WH, Cheng V. Zinc in hair and serum of obese individuals in Taiwan. Am J Clin Nutr. (1988) 48:1307–9. 10.1093/ajcn/48.5.1307 [PubMed] [CrossRef] [Google Scholar]
66. Di Martino G, Matera MG, De Martino B, Vacca C, Di Martino S, Rossi F. Relationship between zinc and obesity. J Med. (1992) 24:177–83. [PubMed] [Google Scholar]
67. Marreiro DN, Fisberg M, Cozzolino SM. Zinc nutritional status in obese children and adolescents. Biol Trace Elem Res. (2002) 86:107–22. 10.1385/bter:86:2:107 [PubMed] [CrossRef] [Google Scholar]
68. Ozata M, Mergen M, Oktenli C, Aydin A, Sanisoglu SY, Bolu E, et al.. Increased oxidative stress and hypozincemia in male obesity. Clin Biochem. (2002) 35:627–31. 10.1016/s0009-9120(02)00363-6 [PubMed] [CrossRef] [Google Scholar]
69. Pisano M, Hilas O. Zinc and taste disturbances in older adults: a review of the literature. Consult Pharm. (2016) 31:267–70. 10.4140/TCP.n.2016.267 [PubMed] [CrossRef] [Google Scholar]
70. Meunier N, O'Connor JM, Maiani G, Cashman KD, Secker DL, Ferry M, et al. Importance of zinc in the elderly: the ZENITH study. Eur J Clin Nutr. (2005) 59(Suppl. 2):S1–4. 10.1038/sj.ejcn.1602286 [PubMed] [CrossRef] [Google Scholar]
71. Haase H, Rink L. The immune system and the impact of zinc during aging. Immun Ageing. (2009) 6:9. 10.1186/1742-4933-6-9 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
72. Mahajan SK, Prasad AS, Lambujon J, Abbasi AA, Briggs WA, McDonald FD. Improvement of uremic hypogeusia by zinc: a double-blind study. Am J Clin Nutr. (1980) 33:1517–21. 10.1093/ajcn/33.7.1517 [PubMed] [CrossRef] [Google Scholar]
73. Eggert JV, Siegler RL, Edomkesmalee E. Zinc supplementation in chronic renal failure. Int J Pediatr Nephrol. (1982) 3:21–4. [PubMed] [Google Scholar]
74. Mahajan SK, Prasad AS, Rabbani P, Briggs WA, McDonald FD. Zinc deficiency: a reversible complication of uremia. Am J Clin Nutr. (1982) 36:1177–83. 10.1093/ajcn/36.6.1177 [PubMed] [CrossRef] [Google Scholar]
75. Gruver AL, Hudson LL, Sempowski GD. Immunosenescence of ageing. J Pathol. (2007) 211:144–56. 10.1002/path.2104 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
76. Wong CP, Magnusson KR, Ho E. Increased inflammatory response in aged mice is associated with age-related zinc deficiency and zinc transporter dysregulation. J Nutr Biochem. (2013) 24:353–9. 10.1016/j.jnutbio.2012.07.005 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
77. Wang X, Valenzano MC, Mercado JM, Zurbach EP, Mullin JM. Zinc supplementation modifies tight junctions and alters barrier function of CACO-2 human intestinal epithelial layers. Dig Dis Sci. (2013) 58:77–87. 10.1007/s10620-012-2328-8 [PubMed] [CrossRef] [Google Scholar]
78. Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. (2020) 51:843–51. 10.1111/apt.15731 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
79. D'Amico F, Baumgart DC, Danese S, Peyrin-Biroulet L. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention and management. Clin Gastroenterol Hepatol. (2020) 18:1663–72. 10.1016/j.cgh.2020.04.001 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
80. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. 10.1016/S0140-6736(20)30183-5 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
81. Pan L. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. (2020) 115:766–73. 10.14309/ajg.0000000000000620 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
82. Bhatnagar S, Natchu UC. Zinc in child health and disease. Indian J Pediatr. (2004) 71:991–5. 10.1007/BF02828114 [PubMed] [CrossRef] [Google Scholar]
83. Lazzerini M. Oral zinc provision in acute diarrhea. Curr Opin Clin Nutr Metab Care. (2016) 19:239–43. 10.1097/MCO.0000000000000276 [PubMed] [CrossRef] [Google Scholar]
84. World Health Organization The Treatment of Diarrhoea: A Manual for Physicians and Other Senior Health Workers. Geneva: WHO; (2005). [Google Scholar]
85. Nataro JP, Yikang D, Yingkang D, Walker K. AggR, a transcriptional activator of aggregative adherence fimbria I expression in enteroaggregative Escherichia coli. J Bacteriol. (1994) 176:4691–9. [PMC free article] [PubMed] [Google Scholar]
86. Medeiros P, Bolick DT, Roche JK, Noronha F, Pinheiro C, Kolling GL, et al.. The micronutrient zinc inhibits EAEC strain 042 adherence, biofilm formation, virulence gene expression, and epithelial cytokine responses benefiting the infected host. Virulence. (2013) 4:624–33. 10.4161/viru.26120 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
87. Aggarwal R, Sentz J, Miller MA. Role of zinc administration in prevention of childhood diarrhea and respiratory illnesses: a meta-analysis. Pediatrics. (2007) 119:1120–30. 10.1542/peds.2006-3481 [PubMed] [CrossRef] [Google Scholar]
88. Roth DE, Richard SA, Black RE. Zinc supplementation for the prevention of acute lower respiratory infection in children in developing countries: meta-analysis and meta-regression of randomized trials. Int J Epidemiol. (2010) 39:795–808. 10.1093/ije/dyp391 [PubMed] [CrossRef] [Google Scholar]
89. Awotiwon AA, Oduwole O, Sinha A, Okwundu CI. Zinc supplementation for the treatment of measles in children. Cochrane Database Syst Rev. (2017) 6:CD011177. 10.1002/14651858.CD011177.pub3 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
90. Prasad AS, Fitzgerald JT, Bao B, Beck FW, Chandrasekar PH. Duration of symptoms and plasma cytokine levels in patients with the common cold treated with zinc acetate. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. (2000) 133:245–52. 10.7326/0003-4819-133-4-200008150-00006 [PubMed] [CrossRef] [Google Scholar]
91. Hemila H, Chalker E. The effectiveness of high dose zinc acetate lozenges on various common cold symptoms: a meta-analysis. BMC Fam Pract. (2015) 16:24. 10.1186/s12875-015-0237-6 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
92. Hemila H, Petrus EJ, Fitzgerald JT, Prasad A. Zinc acetate lozenges for treating the common cold: an individual patient data meta-analysis. Br J Clin Pharmacol. (2016) 82:1393–8. 10.1111/bcp.13057 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
93. Finzi E. Treatment of SARS-CoV-2 with high dose oral zinc salts: A report on four patients. Int J Infect Dis. (2020) 99:307–9. 10.1016/j.ijid.2020.06.006 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
94. Yao JS, Paguio JA, Dee EC, Tan HC, Moulick A, Milazzo C, et al.. The minimal effect of zinc on the survival of hospitalized patients with COVID-19: an observational study. Chest. (2020). 10.1016/j.chest.2020.06.082. [Epub ahead of print]. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
95. Carr AC, Maggini S. Vitamin C and Immune Function. Nutrients. (2017) 9:1211. 10.3390/nu9111211 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
96. Carr A, Frei B. Does vitamin C act as a pro-oxidant under physiological conditions? FASEB J. (1999) 13:1007–24. 10.1096/fasebj.13.9.1007 [PubMed] [CrossRef] [Google Scholar]
97. Englard S, Seifter S. The biochemical functions of ascorbic acid. Annu Rev Nutr. (1986) 6:365–406. 10.1146/annurev.nu.06.070186.002053 [PubMed] [CrossRef] [Google Scholar]
98. Carr AC, Shaw GM, Fowler AA, Natarajan R. Ascorbate-dependent vasopressor synthesis: a rationale for vitamin C administration in severe sepsis and septic shock? Crit Care. (2015) 19:418. 10.1186/s13054-015-1131-2 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
99. Young JI, Zuchner S, Wang G. Regulation of the Epigenome by Vitamin C. Annu Rev Nutr. (2015) 35:545–64. 10.1146/annurev-nutr-071714-034228 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
100. Burr ML, Elwood PC, Hole DJ, Hurley RJ, Hughes RE. Plasma and leukocyte ascorbic acid levels in the elderly. Am J Clin Nutr. (1974) 27:144–51. 10.1093/ajcn/27.2.144 [PubMed] [CrossRef] [Google Scholar]
101. Schorah CJ. The level of vitamin C reserves required in man: towards a solution to the controversy. Proc Nutr Soc. (1981) 40:147–54. 10.1079/pns19810023 [PubMed] [CrossRef] [Google Scholar]
102. Hanck A. Vitamin C in the elderly. Int J Vitam Nutr Res Suppl. (1983) 24:257–69. [PubMed] [Google Scholar]
103. Thurman JE, Mooradian AD. Vitamin supplementation therapy in the elderly. Drugs Aging. (1997) 11:433–49. 10.2165/00002512-199711060-00003 [PubMed] [CrossRef] [Google Scholar]
104. Fletcher AE, Breeze E, Shetty PS. Antioxidant vitamins and mortality in older persons: findings from the nutrition add-on study to the Medical Research Council Trial of Assessment and Management of Older People in the Community. Am J Clin Nutr. (2003) 78:999–1010. 10.1093/ajcn/78.5.999 [PubMed] [CrossRef] [Google Scholar]
105. Hunt C, Chakravorty NK, Annan G. The clinical and biochemical effects of vitamin C supplementation in short-stay hospitalized geriatric patients. Int J Vitam Nutr Res. (1984) 54:65–74. [PubMed] [Google Scholar]
106. Arvinte C, Singh M, Marik PE. Serum levels of vitamin C and vitamin D in a Cohort of Critically Ill COVID-19 Patients of a North American Community Hospital Intensive Care Unit in May 2020: a pilot study. Med Drug Discov. (2020) 8:100064. 10.1016/j.medidd.2020.100064 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
107. Hemila H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. (2013) 31:CD000980 10.1002/14651858.CD000980.pub4 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
108. Uchida K, Mitsui M, Kawakishi S. Monooxygenation of N-acetylhistamine mediated by L-ascorbate. Biochim Biophys Acta. (1989) 991:377–9. 10.1016/0304-4165(89)90131-1 [PubMed] [CrossRef] [Google Scholar]
109. Hunt C, Chakravorty NK, Annan G, Habibzadeh N, Schorah CJ. The clinical effects of vitamin C supplementation in elderly hospitalised patients with acute respiratory infections. Int J Vitam Nutr Res. (1994) 64:212–9. [PubMed] [Google Scholar]
110. Bharara A, Grossman C, Grinnan D, Syed A, Fisher B, DeWilde C, et al.. Intravenous vitamin C administered as adjunctive therapy for recurrent acute respiratory distress syndrome. Case Rep Crit Care. (2016) 2016:8560871. 10.1155/2016/8560871 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
111. Fowler AA, Kim C, Lepler L, Malhotra R, Debesa O, Natarajan R, et al. Intravenous vitamin C as adjunctive therapy for enterovirus/rhinovirus induced acute respiratory distress syndrome. World J Crit Care Med. (2017) 6:85–90. 10.5492/wjccm.v6.i1.85 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
112. Hoang BX, Shaw DG, Fang W, Han B. A Possible application of high dose vitamin C in the prevention and therapy for Coronavirus Infections. J Glob Antimicrob Resist. (2020) 23:256–62. 10.1016/j.jgar.2020.09.025 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
113. Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers. (2019) 5:18 10.1038/s41572-019-0069-0 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
114. Fisher BJ, Kraskauskas D, Martin EJ, Farkas D, Wegelin JA, Brophy D, et al.. Mechanisms of attenuation of abdominal sepsis induced acute lung injury by ascorbic acid. Am J Physiol Lung Cell Mol Physiol. (2012) 303:L20–32. 10.1152/ajplung.00300.2011 [PubMed] [CrossRef] [Google Scholar]
115. Vissers MCM, Wilkie RP. Ascorbate deficiency results in impaired neutrophil apoptosis and clearance and is associated with up-regulation of hypoxia-inducible factor 1alpha. J Leukoc Biol. (2007) 81:1236–44. 10.1189/jlb.0806541 [PubMed] [CrossRef] [Google Scholar]
116. Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med. (2020) 20:124–7. 10.7861/clinmed.2019-coron [PMC free article] [PubMed] [CrossRef] [Google Scholar]
117. Hemila H. Vitamin C intake and susceptibility to pneumonia. Pediatr Infect Dis J. (1997) 16:836–7. 10.1097/00006454-199709000-00003 [PubMed] [CrossRef] [Google Scholar]
118. Hemila H, Chalker E. Vitamin C can shorten the length of stay in the ICU: a meta-analysis. Nutrients. (2019) 11:708. 10.3390/nu11040708 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
119. de Melo AF, Homem-de-Mello M. High-dose intravenous vitamin C may help in cytokine storm in severe SARS-CoV-2 infection. Crit Care. (2020) 24:500. 10.1186/s13054-020-03228-3 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
120. Feyaerts AF, Luyten W. Vitamin C as prophylaxis and adjunctive medical treatment for COVID-19? Nutrition. (2020) 79–80:110948. 10.1016/j.nut.2020.110948 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
121. Herold T, Jurinovic V, Arnreich C, Lipworth BJ, Hellmuth JC, von Bergwelt-Baildon M, et al.. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. (2020) 146:128–36 e124. 10.1016/j.jaci.2020.05.008 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
122. Bohm F, Settergren M, Pernow J. Vitamin C blocks vascular dysfunction and release of interleukin-6 induced by endothelin-1 in humans in vivo. Atherosclerosis. (2007) 190:408–15. 10.1016/j.atherosclerosis.2006.02.018 [PubMed] [CrossRef] [Google Scholar]
123. Hiedra R, Lo KB, Elbashabsheh M, Gul F, Wright RM, Albano J, et al.. The use of IV vitamin C for patients with COVID-19: a case series. Expert Rev Anti Infect Ther. (2020) 1–3. 10.1080/14787210.2020.1794819 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
124. Waqas Khan HM, Parikh N, Megala SM, Predeteanu GS. Unusual early recovery of a critical COVID-19 patient after administration of intravenous vitamin C. Am J Case Rep. (2020) 21:e925521. 10.12659/AJCR.925521 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
125. Pludowski P, Holick MF, Pilz S, Wagner CL, Hollis BW, Grant WB, et al.. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-a review of recent evidence. Autoimmun Rev. (2013) 12:976–89. 10.1016/j.autrev.2013.02.004 [PubMed] [CrossRef] [Google Scholar]
126. Catarino AM, Claro C, Viana I. Vitamin D - current perspectives. J Portuguese Soc Dermatol Venereol. (2016) 74:345–53. 10.29021/spdv.74.4.673 [CrossRef] [Google Scholar]
127. Peters BSE, Martini LA. Vitamina D, funções plenamente reconhecidas de nutrientes. Int Life Sci Instit Brasil. (2014) 2:1–23. [Google Scholar]
128. de Castro LCG. O sistema endocrinológico vitamina D. Arq Bra Endocrinol Metabol. (2011) 55:566–75. 10.1590/S0004-27302011000800010 [PubMed] [CrossRef] [Google Scholar]
129. Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet. (1982) 1:74–6. 10.1016/s0140-6736(82)90214-8 [PubMed] [CrossRef] [Google Scholar]
130. Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. (1987) 64:1165–8. 10.1210/jcem-64-6-1165 [PubMed] [CrossRef] [Google Scholar]
131. Holick MF. Vitamin D deficiency. N Engl J Med. (2007) 357:266–81. 10.1056/NEJMra070553 [PubMed] [CrossRef] [Google Scholar]
132. Holick MF. Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr. (1995) 61(3 Suppl):638S–45S. 10.1093/ajcn/61.3.638S [PubMed] [CrossRef] [Google Scholar]
133. Goring H, Koshuchowa S. Vitamin D – the sun hormone. Life in environmental mismatch. Biochemistry. (2015) 80:8–20. 10.1134/S0006297915010022 [PubMed] [CrossRef] [Google Scholar]
134. Vanherwegen AS, Gysemans C, Mathieu C. Regulation of immune function by vitamin D and its use in diseases of immunity. Endocrinol Metab Clin North Am. (2017) 46:1061–94. 10.1016/j.ecl.2017.07.010 [PubMed] [CrossRef] [Google Scholar]
135. Chakhtoura M, Napoli N, El Hajj Fuleihan G. Commentary: myths and facts on vitamin D amidst the COVID-19 pandemic. Metabolism. (2020) 109:154276. 10.1016/j.metabol.2020.154276 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
136. Xu Y, Baylink DJ, Chen CS, Reeves ME, Xiao J, Lacy C, et al.. The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19. J Transl Med. (2020) 18:322. 10.1186/s12967-020-02488-5 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
137. Teymoori-Rad M, Shokri F, Salimi V, Marashi SM. The interplay between vitamin D and viral infections. Rev Med Virol. (2019) 29:e2032. 10.1002/rmv.2032 [PubMed] [CrossRef] [Google Scholar]
138. Klotman ME, Chang TL. Defensins in innate antiviral immunity. Nat Rev Immunol. (2006) 6:447–56. 10.1038/nri1860 [PubMed] [CrossRef] [Google Scholar]
139. Crane-Godreau MA, Clem KJ, Payne P, Fiering S. Vitamin D deficiency and air pollution exacerbate COVID-19 through suppression of antiviral peptide LL37. Front Public Health. (2020) 8:232. 10.3389/fpubh.2020.00232 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
140. Munshi R, Hussein MH, Toraih EA, Elshazli RM, Jardak C, Sultana N, et al.. Vitamin D insufficiency as a potential culprit in critical COVID-19 patients. J Med Virol. (2020). 10.1002/jmv.26360. [Epub ahead of print]. [PubMed] [CrossRef] [Google Scholar]
141. Orru B, Szekeres-Bartho J, Bizzarri M, Spiga AM, Unfer V. Inhibitory effects of Vitamin D on inflammation and IL-6 release. A further support for COVID-19 management? Eur Rev Med Pharmacol Sci. (2020) 24:8187–93. 10.26355/eurrev_202008_22507 [PubMed] [CrossRef] [Google Scholar]
142. Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. The possible role of Vitamin D in suppressing cytokine storm and associated mortality in COVID-19 Patients. medRxiv. (2020) 2020.2004.2008.20058578. 10.1101/2020.04.08.20058578 [CrossRef] [Google Scholar]
143. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al.. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. (2017) 356:i6583. 10.1136/bmj.i6583 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
144. Clairmont A, Tessman D, Stock A, Nicolai S, Stahl W, Sies H. Induction of gap junctional intercellular communication by vitamin D in human skin fibroblasts is dependent on the nuclear Induction of gap junctional intercellular communication by vitamin D in human skin fibroblasts is dependent on the nuclear vitamin D receptor. Carcinogenesis. (1996) 17:1389–91. 10.1093/carcin/17.6.1389 [PubMed] [CrossRef] [Google Scholar]
145. Gniadecki R, Gajkowska B, Hansen M. 1,25-dihydroxyvitamin D3 stimulates the assembly of adherens junctions in keratinocytes: involvement of protein kinase C. Endocrinology. (1997) 138:2241–8. 10.1210/endo.138.6.5156 [PubMed] [CrossRef] [Google Scholar]
146. Chen H, Lu R, Zhang YG, Sun J. Vitamin D receptor deletion leads to the destruction of tight and adherens junctions in lungs. Tissue Barriers. (2018) 6:1–13. 10.1080/21688370.2018.1540904 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
147. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al.. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:1911–30. 10.1210/jc.2011-0385 [PubMed] [CrossRef] [Google Scholar]
148. Braiman M. Latitude Dependence of the COVID-19 Mortality Rate — A Possible Relationship to Vitamin D Deficiency? New York, NY: Syracuse University Department of Chemistry; (2020). 10.2139/ssrn.3561958 [CrossRef] [Google Scholar]
149. Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. (2020) 32:1195–8. 10.1007/s40520-020-01570-8 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
150. Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, et al.. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. (2020) 287:3693–702. 10.1111/febs.15495 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
151. Panarese A, Shahini E. Letter: Covid-19, and vitamin D. Aliment Pharmacol Ther. (2020) 51:993–5. 10.1111/apt.15752 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
152. Rhodes JM, Subramanian S, Laird E, Kenny RA. Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity. Aliment Pharmacol Ther. (2020) 51:1434–7. 10.1111/apt.15777 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
153. Valcour A, Blocki F, Hawkins DM, Rao SD. Effects of age and serum 25-OH-vitamin D on serum parathyroid hormone levels. J Clin Endocrinol Metab. (2012) 97:3989–95. 10.1210/jc.2012-2276 [PubMed] [CrossRef] [Google Scholar]
154. Amrein K, Venkatesh B. Vitamin D and the critically ill patient. Curr Opin Clin Nutr Metab Care. (2012) 15:188–93. 10.1097/MCO.0b013e32834f0027 [PubMed] [CrossRef] [Google Scholar]
155. Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Wetterslev J, Simonetti RG, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev. (2014) 10:CD007470 10.1002/14651858.CD007470.pub3 [PubMed] [CrossRef] [Google Scholar]
156. Lippi G, Henry BM, Bovo C, Sanchis-Gomar F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis (Berl). (2020) 7:85–90. 10.1515/dx-2020-0041 [PubMed] [CrossRef] [Google Scholar]
157. Xu J, Yang J, Chen J, Luo Q, Zhang Q, Zhang H. Vitamin D alleviates lipopolysaccharideinduced acute lung injury via regulation of the reninangiotensin system. Mol Med Rep. (2017) 16:7432–8. 10.3892/mmr.2017.7546 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
158. Kumar D, Gupta P, Banerjee D. Letter: does vitamin D have a potential role against COVID-19? Aliment Pharmacol Ther. (2020) 52:409–11. 10.1111/apt.15801 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
159. Malek Mahdavi A. A brief review of interplay between vitamin D and angiotensin-converting enzyme 2: implications for a potential treatment for COVID-19. Rev Med Virol. (2020) 30:e2119. 10.1002/rmv.2119 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
160. Musavi H, Abazari O, Barartabar Z, Kalaki-Jouybari F, Hemmati-Dinarvand M, Esmaeili P, et al.. The benefits of Vitamin D in the COVID-19 pandemic: biochemical and immunological mechanisms. Arch Physiol Biochem. (2020). 10.1080/13813455.2020.1826530. [Epub ahead of print]. [PubMed] [CrossRef] [Google Scholar]
161. Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA. Perspective: Vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J Intern Med. (2020). 10.1111/joim.13149. [Epub ahead of print]. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
162. Patel AB, Verma A. COVID-19 Angiotensin-converting enzyme inhibitors angiotensin receptor blockers: what is the evidence? JAMA. (2020) 323:1769–70. 10.1001/jama.2020.4812 [PubMed] [CrossRef] [Google Scholar]
163. Ebadi M, Montano-Loza AJ. Perspective: improving vitamin D status in the management of COVID-19. Eur J Clin Nutr. (2020) 74:856–9. 10.1038/s41430-020-0661-0 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
164. Siuka D, Pfeifer M, Pinter B. Vitamin D supplementation during the COVID-19 pandemic. Mayo Clin Proc. (2020) 95:1804–5. 10.1016/j.mayocp.2020.05.036 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
165. Weir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the severity of COVID-19? Clin Med. (2020) 20:e107–8. 10.7861/clinmed.2020-0301 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
166. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al.. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. (2020) 382:1564–7. 10.1056/NEJMc2004973 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
167. Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al.. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. (2020) 12:372. 10.3390/v12040372 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
168. Li JO, Lam DSC, Chen Y, Ting DSW. Novel Coronavirus disease 2019 (COVID-19): The importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. (2020) 104:297–8. 10.1136/bjophthalmol-2020-315994 [PubMed] [CrossRef] [Google Scholar]
169. Li JY, You Z, Wang Q, Zhou ZJ, Qiu Y, Luo R, et al.. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microbes Infect. (2020) 22:80–5. 10.1016/j.micinf.2020.02.002 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
170. Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. (2020) 395:e39. 10.1016/S0140-6736(20)30313-5 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
171. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. 10.1016/S0140-6736(20)30185-9 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
172. Zihni C, Mills C, Matter K, Balda MS. Tight junctions: from simple barriers to multifunctional molecular gates. Nat Rev Mol Cell Biol. (2016) 17:564–80. 10.1038/nrm.2016.80 [PubMed] [CrossRef] [Google Scholar]
173. Alberts B, Bray D, Watson J. Biologia Molecular da Célula. Artmed; (2017). [Google Scholar]
174. Laukoetter MG, Bruewer M, Nusrat A. Regulation of the intestinal epithelial barrier by the apical junctional complex. Curr Opin Gastroenterol. (2006) 22:85–9. 10.1097/01.mog.0000203864.48255.4f [PubMed] [CrossRef] [Google Scholar]
175. Zhang YG, Wu S, Sun J. Vitamin D. Vitamin D receptor, and tissue barriers. Tissue Barriers. (2013) 1:e23118. 10.4161/tisb.23118 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
176. Miyoshi Y, Tanabe S, Suzuki T. Cellular zinc is required for intestinal epithelial barrier maintenance via the regulation of claudin-3 and occludin expression. Am J Physiol Gastrointest Liver Physiol. (2016) 311:105–16. 10.1152/ajpgi.00405.2015 [PubMed] [CrossRef] [Google Scholar]
177. Campbell HK, Maiers JL, DeMali KA. Interplay between tight junctions & adherens junctions. Exp Cell Res. (2017) 358:39–44. 10.1016/j.yexcr.2017.03.061 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
178. Green KJ, Jaiganesh A, Broussard JA. Desmosomes: essential contributors to an integrated intercellular junction network. F1000Res. (2019) 8. 10.12688/f1000research.20942.1 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
179. Bergelson JM. Intercellular junctional proteins as receptors and barriers to virus infection and spread. Cell Host Microbe. (2009) 5:517–21. 10.1016/j.chom.2009.05.009 [PubMed] [CrossRef] [Google Scholar]
180. Teoh KT, Siu YL, Chan WL, Schluter MA, Liu CJ, Peiris JS, et al.. The SARS coronavirus E protein interacts with PALS1 and alters tight junction formation and epithelial morphogenesis. Mol Biol Cell. (2010) 21:3838–52. 10.1091/mbc.E10-04-0338 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
181. Sturniolo GC, Di Leo V, Ferronato A, D'Odorico A, D'Inca R. Zinc supplementation tightens “leaky gut” in Crohn's disease. Inflamm Bowel Dis. (2001) 7:94–8. 10.1097/00054725-200105000-00003 [PubMed] [CrossRef] [Google Scholar]
182. Tran CD, Ball JM, Sundar S, Coyle P, Howarth GS. The role of zinc and metallothionein in the dextran sulfate sodium-induced colitis mouse model. Dig Dis Sci. (2007) 52:2113–21. 10.1007/s10620-007-9765-9 [PubMed] [CrossRef] [Google Scholar]
183. Zhang B, Guo Y. Supplemental zinc reduced intestinal permeability by enhancing occludin and zonula occludens protein-1 (ZO-1) expression in weaning piglets. Br J Nutr. (2009) 102:687–93. 10.1017/S0007114509289033 [PubMed] [CrossRef] [Google Scholar]
184. Garcia-Hernandez V, Quiros M, Nusrat A. Intestinal epithelial claudins: expression and regulation in homeostasis and inflammation. Ann N Y Acad Sci. (2017) 1397:66–79. 10.1111/nyas.13360 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
185. Atisook K, Carlson S, Madara JL. Effects of phlorizin and sodium on glucose-elicited alterations of cell junctions in intestinal epithelia. Am J Physiol. (1990) 258:C77–85. 10.1152/ajpcell.1990.258.1.C77 [PubMed] [CrossRef] [Google Scholar]
186. Reyes JL, Lamas M, Martin D, del Carmen Namorado M, Islas S, Luna J, et al.. The renal segmental distribution of claudins changes with development. Kidney Int. (2002) 62:476–87. 10.1046/j.1523-1755.2002.00479.x [PubMed] [CrossRef] [Google Scholar]
187. Escaffit F, Boudreau F, Beaulieu JF. Differential expression of claudin-2 along the human intestine: implication of GATA-4 in the maintenance of claudin-2 in differentiating cells. J Cell Physiol. (2005) 203:15–26. 10.1002/jcp.20189 [PubMed] [CrossRef] [Google Scholar]
188. Van Itallie CM, Anderson JM. Claudins and epithelial paracellular transport. Annu Rev Physiol. (2006) 68:403–29. 10.1146/annurev.physiol.68.040104.131404 [PubMed] [CrossRef] [Google Scholar]
189. Bao S, Knoell DL. Zinc modulates cytokine-induced lung epithelial cell barrier permeability. Am J Physiol Lung Cell Mol Physiol. (2006) 291:L1132–1141. 10.1152/ajplung.00207.2006 [PubMed] [CrossRef] [Google Scholar]
190. Oudemans-van Straaten HM, Spoelstra-de Man AM, de Waard MC. Vitamin C revisited. Crit Care. (2014) 18:460. 10.1186/s13054-014-0460-x [PMC free article] [PubMed] [CrossRef] [Google Scholar]
191. Berger MM, Oudemans-van Straaten HM. Vitamin C supplementation in the critically ill patient. Curr Opin Clin Nutr Metab Care. (2015) 18:193–201. 10.1097/MCO.0000000000000148 [PubMed] [CrossRef] [Google Scholar]
192. Rao R. Occludin phosphorylation in regulation of epithelial tight junctions. Ann N Y Acad Sci. (2009) 1165:62–8. 10.1111/j.1749-6632.2009.04054.x [PMC free article] [PubMed] [CrossRef] [Google Scholar]
193. Fujita H, Sugimoto K, Inatomi S. Tight junction proteins claudin-2 and−12 are critical for Vitamin D-dependent Ca2 absorption between enterocytes. Molecular Biol Cell. (2008) 19:1912–21. 10.1091/mbc.e07-09-0973 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
194. Yin Z, Pintea V, Lin Y, Hammock BD, Watsky MA. Vitamin D enhances corneal epithelial barrier function. Invest Ophthalmol Vis Sci. (2011) 52:7359–64. 10.1167/iovs.11-7605 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
195. Palmer HG, Gonzalez-Sancho JM, Espada J, Berciano MT, Puig I, Baulida J, et al.. Vitamin D(3) promotes the differentiation of colon carcinoma cells by the induction of E-cadherin and the inhibition of beta-catenin signaling. J Cell Biol. (2001) 154:369–87. 10.1083/jcb.200102028 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
196. Takeichi M. Morphogenetic roles of classic cadherins. Curr Opin Cell Biol. (1995) 7:619–27. 10.1016/0955-0674(95)80102-2 [PubMed] [CrossRef] [Google Scholar]
197. Gumbiner BM. Cell adhesion: the molecular basis of tissue architecture and morphogenesis. Cell. (1996) 84:345–57. 10.1016/s0092-8674(00)81279-9 [PubMed] [CrossRef] [Google Scholar]
198. Birchmeier W, Behrens J. Cadherin expression in carcinomas: role in the formation of cell junctions and the prevention of invasiveness. Biochim Biophys Acta. (1994) 1198:11–26. 10.1016/0304-419x(94)90003-5 [PubMed] [CrossRef] [Google Scholar]
199. Perl AK, Wilgenbus P, Dahl U, Semb H, Christofori G. A causal role for E-cadherin in the transition from adenoma to carcinoma. Nature. (1998) 392:190–3. 10.1038/32433 [PubMed] [CrossRef] [Google Scholar]
200. Christofori G, Semb H. The role of the cell-adhesion molecule E-cadherin as a tumour-suppressor gene. Trends Biochem Sci. (1999) 24:73–6. 10.1016/s0968-0004(98)01343-7 [PubMed] [CrossRef]